Research
Meet our researchers: Dr Sandy Hung
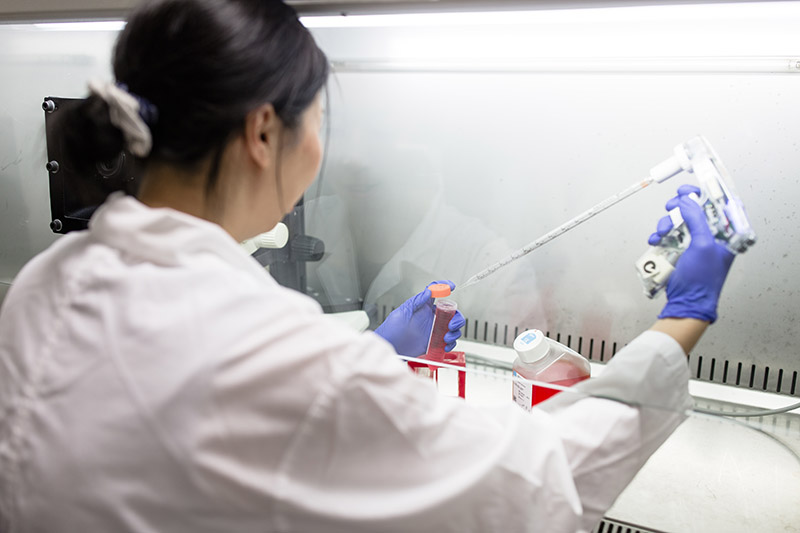
Dr Sandy Hung is a Research Fellow in CERA’s Clinical Genetics team working to develop gene delivery technology to improve current treatments for inherited retinal disease – a leading cause of blindness in working-age Australians.
What motivated you to get into science?
When I was young, a close family member was diagnosed with cancer, and I was motivated to get into science.
I studied an undergraduate degree in biomedical science, majoring in cancer biology and moved to Melbourne to do my PhD at the Peter MacCallum Cancer Centre, where I studied cell growth.
I completed my postdoctoral training at the at the University of California, Irvine, studying mechanisms of cell growth in yeast, and later moved to work in stem cell research at the National Institute of Aging.
What inspired you to pursue rare eye disease research?
Being a more clinically based institute, CERA differed to the previous laboratory environments I worked in.
We got to hear more of the stories of patients and how eye diseases affected their everyday lives. This really inspired me to push my research forward, especially in times where I met difficulties or challenges in my experiments.
I work in Professor Alex Hewitt’s Clinical Genetics Unit, which is focused on finding new treatments for patients with inherited retinal diseases (IRDs).
Professor Hewitt sees many patients at his clinic with rare diseases caused by different genetic ‘mistakes’ that cause different cell types of the retina to not function properly.
In one of my earlier projects, my role was using the latest gene editing techniques to try and correct the mistakes that cause these diseases using stem cell models that were derived from the patient’s skin cells.
During this project, I was fortunate to meet some of the patient advocates and gained a better understanding of how important the work in the laboratory was to help develop treatments for them.
Around this time, my colleague Dr Sandra Staffieri AO took me to the Royal Children’s Hospital and showed me the work she does as Retinoblastoma Care Coordinator – supervising the team administering treatments to children living with a rare eye cancer called retinoblastoma.
I’d never actually stepped into a clinical setting prior to this, and it was so different to the work we do in the laboratory.
I got to see first-hand the limitations of the currently available treatments. And it really drove home the importance of the work we’re doing and how it could make a difference.
The second encounter was meeting a young boy living with Usher Syndrome – a condition causing hearing and vision loss, and sometimes loss of balance.
His family asked to meet the researchers working on treatments, and we showed them around the lab. They were very passionate about advocating for Usher, which was very inspiring to see.
When I’m working on related projects in the lab, and especially during challenging times, I often think of these encounters which help motivate me to try harder and to push for the work we do.
Why is it so important to study rare diseases?
Different IRDs or genetic mistakes can cause the different cell types in our light-sensing retina to not function properly, which can eventually lead to irreversible vision loss.
Our Clinical Genetics Unit is aiming to develop tools that can lead to personalised treatments for different rare eye diseases. Even though we are currently working only on a few particular IRDs, the technology can be adapted to target other genetic mistakes in other IRDs.
Currently, many of the gene editing tools we can use to correct genetic mistakes are too big to fit in currently available gene delivery systems. Or they don’t target the right cells in the light-sensing retina at the back of our eye.
One of the projects that our group is working on is to adapt a bigger gene delivery vehicle to target the affected cells in the retina more effectively. And the first cell type we’re targeting is photoreceptors.
If we’re successful, we hope to treat IRDs such as retinitis pigmentosa. And eventually, we could target different cell types and potentially treat even more diseases.
What is the best part of working at CERA?
I feel really grateful to have the opportunity and freedom to develop and work on research that could potentially lead to outcomes that make a real difference to people living with eye disease. It really gives me a purpose in the work that I get to do.
