This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Research
Boost for glaucoma research
Pioneering research into blood supply and optic nerve damage in glaucoma has received a major boost from Fighting Blindness Canada.
Dr Luis Alarcon-Martinez was part of the research team which discovered microscopic structures in the retina which could hold the key to preventing vision loss from glaucoma.
Now a Transformative Research Grant from Fighting Blindness Canada will see him lead an international collaboration from CERA to further advance that research in search of new treatment for the world’s leading cause of irreversible blindness.
Dr Alarcon-Martinez, the Head of Visual Neurovascular Research, CERA’s Head of Glaucoma Research Professor Keith Martin, Professor Adriana Di Polo from the University of Montreal and Professor Bang Bui from the University of Melbourne’s Department of Optometry and Vision Sciences are co-investigators on the new study.
“We are extremely grateful to Fighting Blindness Canada for supporting our research,’’ says Dr Alarcon-Martinez.
“We hope our new study will enable us to gain a deeper understanding of the processes which control blood flow to cells in the retina to prevent damage and protect sight.
“A better understanding of how the retina and optic nerve works also increases our knowledge of the cardiovascular system and brain.
“In addition to glaucoma, findings of our research could also be applied to other conditions that damage the retina, optic nerve and brain including diabetic retinopathy, retinopathy caused by prematurity, Alzheimer’s disease, Parkinson’s disease and motor neurone disease.’’
How our vision works
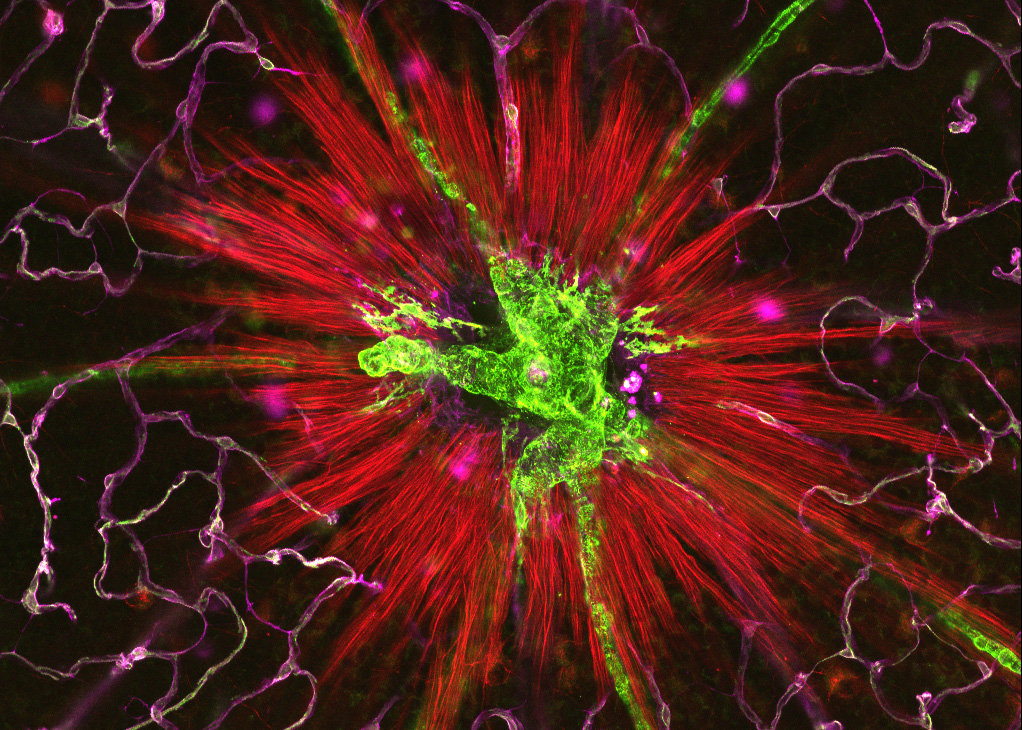
Our vision relies on the successful function of millions of cells and nerve fibres that make up the retina and optic nerve which connects the eye to the brain.
Light is picked up in the retina – a layer of light sensing cells at the back of the eye – and then turned into electrical signals by retinal ganglion cells which transmit visual information to the brain via long nerve fibres which bundle together to make up the optic nerve.
To work properly, retinal ganglion cells need a good supply of oxygen and nutrients from nearby blood vessels.
When that supply is disrupted, cell damage and vision loss occurs.
Nanotube discovery
Before moving to CERA in 2021, Dr Alarcon-Martinez was part of a team which discovered a previously unknown mechanism which enables retinal cells to communicate with each other to regulate blood supply.
Embedded within the capillaries are pericytes, cells control the amount of blood passing through the capillaries by dilating or contracting them.
Looking at vascular changes in the retinas of mice, Dr Alarcon-Martinez and colleagues showed that pericytes project very thin tubes – known as nanotubes – to communicate with one another and supply blood where it is most needed.
Their study, published in Nature in 2020 also showed that capillaries lose their ability to regulate blood supply when these nanotubes were damaged. This was supported by further research published in PNAS, the journal of the National Academy of Sciences U.S.A. which also identified that excessive calcium influx could play a role in damaging nanotubes.
New research
The new funding from Fighting Blindness Canada will enable the research team to conduct further research aimed at preventing the damage of these nanotubes.
Using cutting-edge two photon microscopy Dr Alarcon-Martinez will conduct experiments that observe the function of nanotubes in mouse models and trial a number of approaches to stopping the damage.
Professor Keith Martin, who is also leading another research project to develop a gene therapy to strengthen the optic nerve, says the research could transform the understanding of glaucoma and help develop new targets for treatment.
“For many years it’s been thought that impaired blood supply could be a key factor in the optic nerve damage caused by glaucoma and other neurodegenerative diseases,’’ he says.
“But until now, we have not understood how this process works – which is a critical first step in developing a target for the development of new drugs to prevent damage and restore sight.’’
Professor Martin says the findings of the new research project will provide valuable insights to other researchers investigating new therapies for glaucoma. This includes Dr Flora Hui’s clinical trial of vitamin B3 to prevent vision loss from glaucoma and Professor Martin’s own work developing a gene therapy to prevent optic nerve damage.’’
More information
Alarcon-Martinez et al, Pericyte dysfunction and loss of inter-pericyte tunneling nanotubes promote neurovascular deficits in glaucoma, PNAS (2022) https://doi.org/10.1073/pnas.2110329119
Alarcon-Martinez et al, Interpericyte tunnelling nanotubes regulate neurovascular coupling, Nature (2020) https://doi.org/10.1038/s41586-020-2589-x